
Skin conditions are common...

...but they affect more than just a person’s skin

In 2020, the All-Party Parliamentary Group on Skin surveyed 500 patients with skin conditions and found that:2
felt that their condition affected their emotional and psychological wellbeing2

felt that their condition had directly affected their social life and leisure activities2

stated that their condition had affected their sleep2

felt that their condition had negatively affected intimate relationships2
Treat the whole person, not just their symptoms

Treating the skin condition is the first step in management but it doesn’t end there.3 The burden of living with a skin condition impacts multiple areas of life from physical health, such as sleep, through to emotional wellbeing and social functioning.2
A holistic management approach that encompasses all aspects of living with a skin condition, including the patient’s emotional and psychological needs, should be taken to improve patient outcomes and wellbeing.3
Inflammatory skin conditions can cause stress…

Many inflammatory skin conditions, including eczema (or atopic dermatitis), acne, psoriasis and rosacea have been shown to be associated with psychological stress, such as anxiety, depression and suicidal ideation.3–5
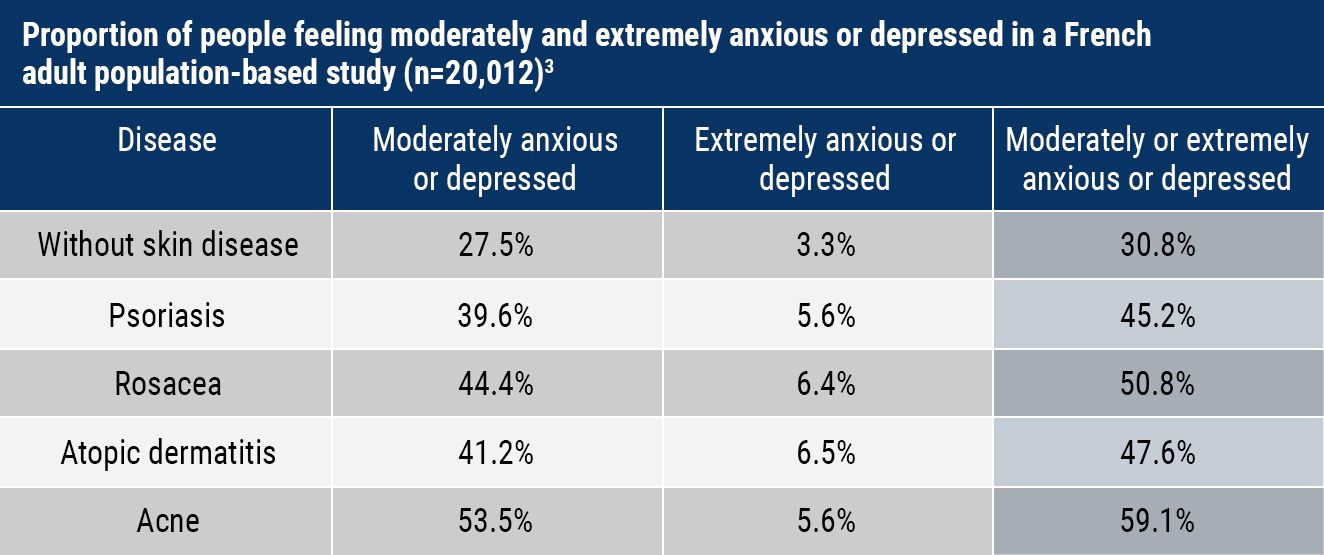
Having a skin condition can distort a patient’s self-image and cause feelings of social isolation, loneliness, low self-esteem and low body satisfaction.4,5
...and stress can trigger or worsen inflammation

Many patients with chronic inflammatory skin conditions such as eczema or rosacea, which have a relapsing and remitting nature, often report stress as a trigger for flare-ups.6–8
Stress can impair skin barrier function, increase inflammation, and induce or exacerbate skin conditions including acne, eczema, psoriasis and rosacea.9,10
Common inflammatory skin conditions

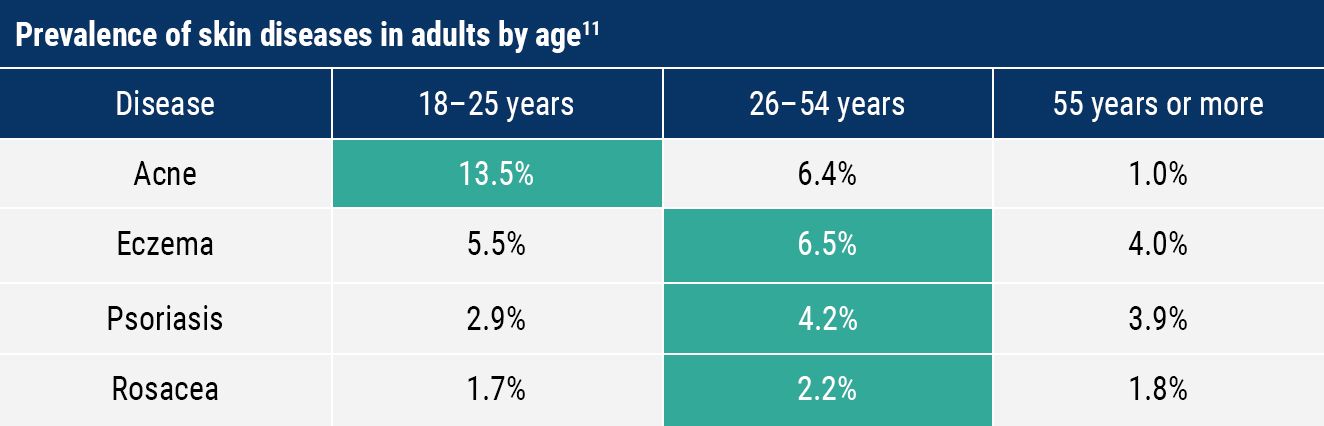
Acne, eczema, psoriasis and rosacea are amongst the top ten most common skin conditions seen in Europe according to a population-based study (n=44,689) carried out between 2021 and 2022 in 27 European countries, including the UK.11
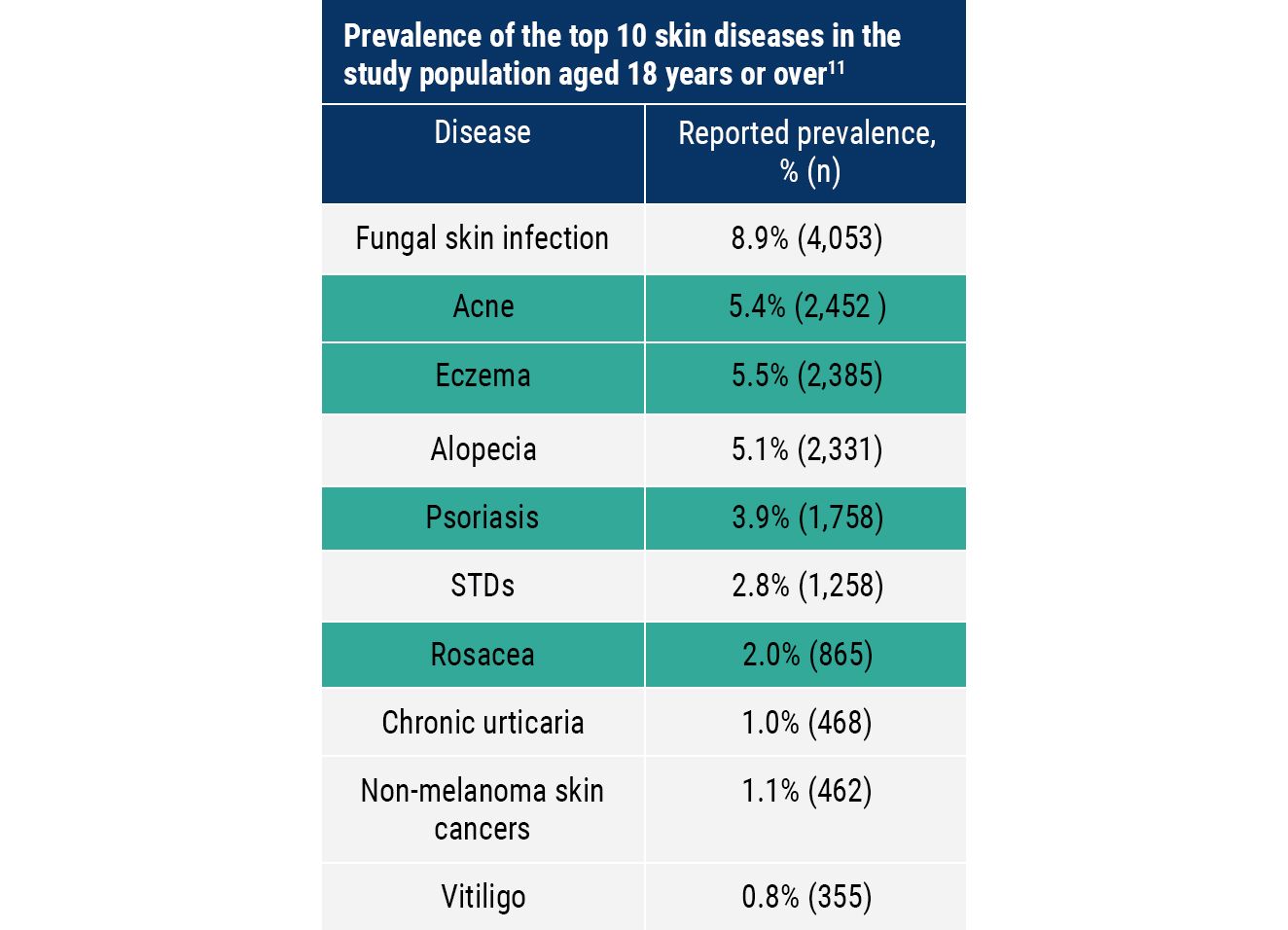
The prevalence of acne in adults was highest in 18–25 year olds.11 However, eczema, psoriasis and rosacea were reported more frequently in 26–54 year olds.11
Where do acne, eczema, psoriasis and rosacea usually appear on the body?

Common sites affected by acne include the face, back and chest12,13
Common sites affected by eczema include the hands, inside of the elbows, back of the knees, face and scalp (in children)14
Common sites affected by psoriasis include the elbows, knees, scalp and lower back15
Common sites affected by rosacea include the nose, cheeks, forehead, chin, neck and chest16,17
Acne

Acne can appear at any age but it is most frequently seen in adolescents.13 Approximately 95% of 11–30 year olds are affected by acne to some degree.13
Acne can cause significant psychological distress by negatively impacting on self-esteem and body image, which can be especially damaging in teenagers and young adults as their sense of self and social identities are being formed.18
Acne can have a lifelong impact on patients if the disease becomes chronic, if there is scarring or if pigmentation changes occur.12,18 Early recognition and a holistic approach to treatment is important to help improve patient outcomes.12
Key diagnostic features12,13
● Spots
● Oily skin
● Hot/painful skin
● Non-inflamed lesions/comedones (blackheads, whiteheads)
● Inflamed lesions (papules, pustules, nodules)
● Scarring
● Pigmentation (especially in black and brown skin)
Common sites12,13
● Face
● Back
● Chest
Treatment options for acne include:19
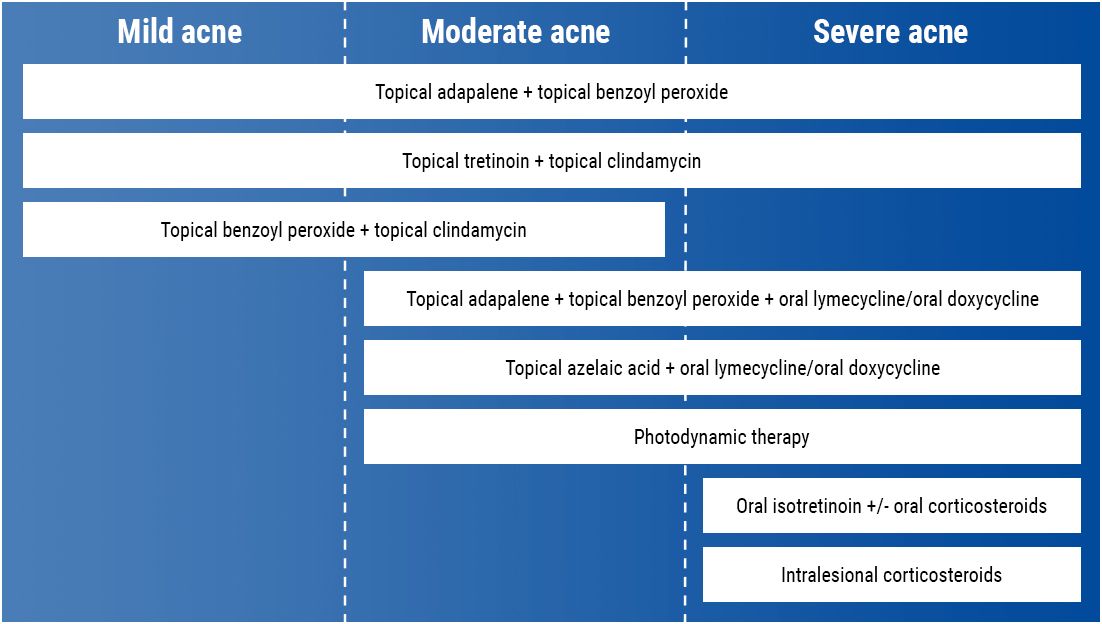
What drugs can be prescribed for acne?
Eczema

Eczema, also known as atopic dermatitis, is most frequently seen in young children before they reach 1 year of age.14 Some children grow out of their eczema as they get older, but typically this is a chronic condition that requires long-term management throughout the patient’s life.14
It is common for children with eczema to develop other allergic conditions including food allergies, allergic rhinitis and asthma – this is referred to as the ‘allergic march’ or ‘atopic march’.20
Living with eczema can be debilitating and exhausting for patients, not only from the physical aspects of disease such as persistent itching which can disturb sleep, but also the psychological burden associated with looking different to other people and feeling embarrassed or ashamed because of it.21
Key diagnostic features14
● Itchy, dry, cracked or sore skin
● Visibly irritated skin in creases of skin
● History of skin irritation
● History of asthma or hay fever
● Small areas of dry skin
● Widespread inflamed skin all over the body
● Inflamed skin may look red on white skin, and darker brown/purple/grey on brown and black skin
Common sites14
● Hands
● Inside of elbows
● Back of the knee
● Face and scalp (in children)
Treatment options include:22
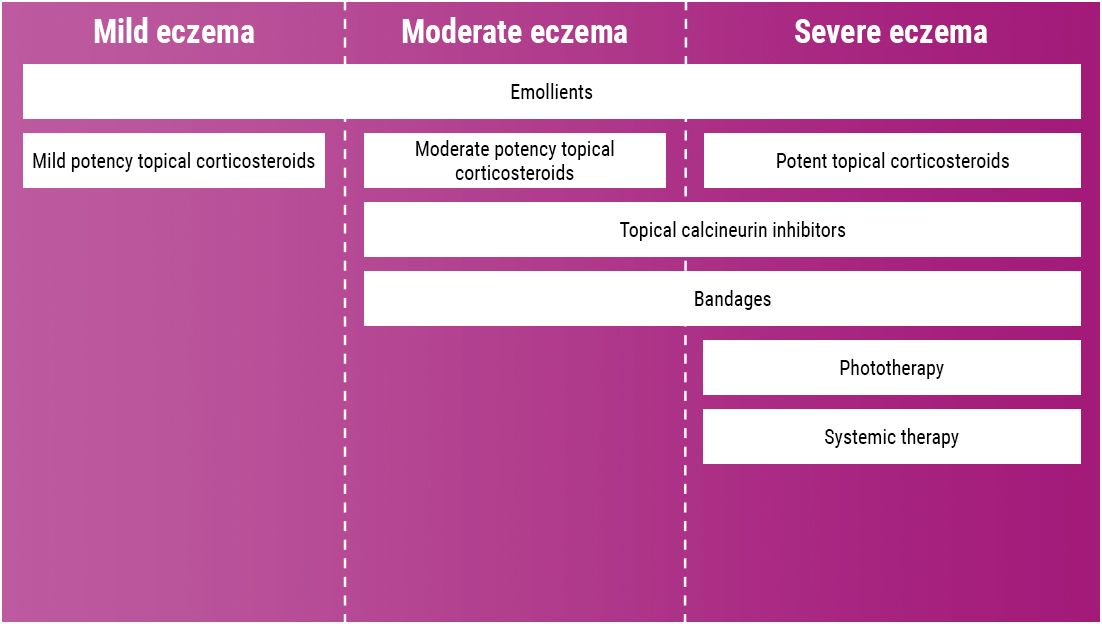
What drugs can be prescribed for eczema?
Psoriasis

Psoriasis can develop at any age but it is most frequently seen in 20–30 year olds and 50–60 year olds.15 It presents as patchy flakes that form scales or ‘plaques’ on the skin, which are a result of excessive skin cell production.15,23
In healthy individuals, the skin replacement process usually takes 3–4 weeks, but in people with psoriasis the process takes only 3–7 days.15 Psoriasis has been shown to increase the risk of other diseases including psoriatic arthritis and cardiovascular disease (CVD).24
It is estimated that psoriatic arthritis affects up to 30% of people with psoriasis.24 Similarly, studies have demonstrated people with psoriasis are up to 50% more likely to develop CVD, with more severe disease relating to higher cardiovascular risk.25 Disease severity can range from mild to to severe; however, psoriasis that appears relatively mild in severity can still bear significant impact on the individual by affecting their self-esteem and quality of life.15
Key diagnostic features15
● Flaky patches of skin which form scales
● Patches can be itchy/sore
● Patches can appear pink/red and scales can appear white/silvery
● In black and brown skin, patches can also look purple/dark brown and scales may appear grey
● In severe cases, skin near joints may crack and bleed
Common sites15
● Elbows
● Knees
● Scalp
● Lower back
Treatment options include:25
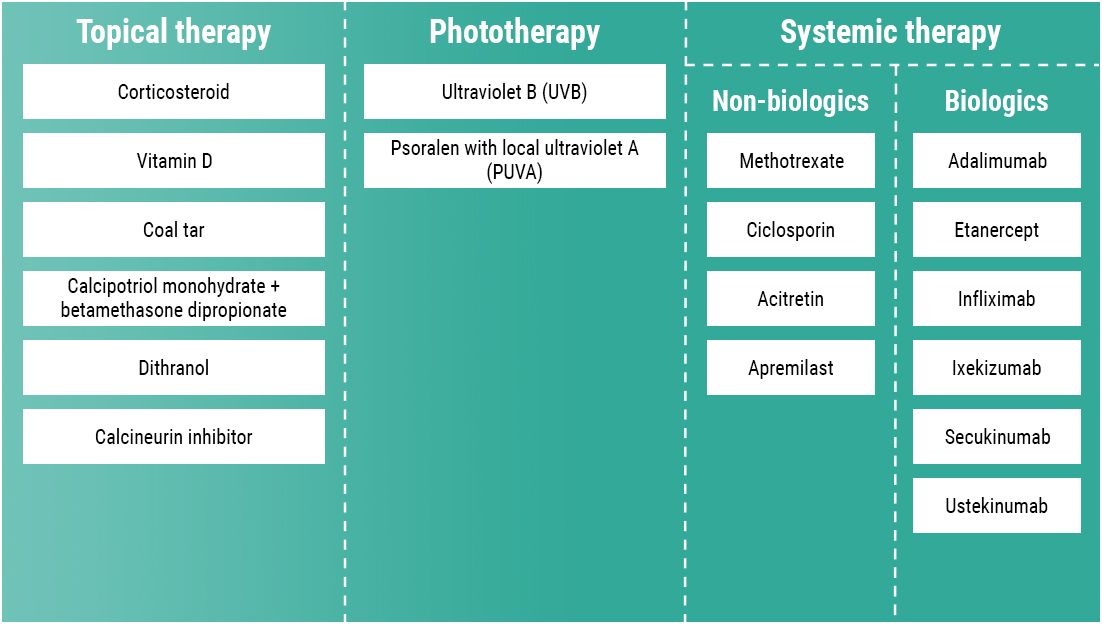
What drugs can be prescribed for psoriasis?


Rosacea

Rosacea is often seen in adults aged between 30–60 years and typically occurs across the middle part of the face.17 The condition usually begins with the person having a tendency to blush easily, which later becomes more frequent and can lead to permanent redness, vasodilatation and bumps on the face.27
More than 50% of people with rosacea will also experience ocular symptoms, which may require referral to an ophthalmologist in some cases.17 There are a number of triggers known to exacerbate rosacea; these include sunlight exposure, stress, spicy food, topical steroids and medications that cause vasodilatation.17,27
Rosacea can have a significant impact on patients’ wellbeing by causing feelings of embarrassment, low self-esteem, anxiety and depression.27
Key diagnostic features16,17
● Redness/blushing (may be difficult to see in black and brown skin) typically across the face that comes and goes, lasting for a few minutes each time
● Often associated with burning/stinging sensation
● Face may feel warm, hot or painful
● Ocular symptoms (gritty eyes, conjunctivitis, episcleritis, chalazion)
● Telangiectasia
● Papules
● Pustules
● Absence of open comedones (blackheads)
● Thickening of skin if condition becomes chronic
Common sites16,17
● Nose
● Cheeks
● Forehead
● Chin
● Neck
● Chest
Treatment options include:28
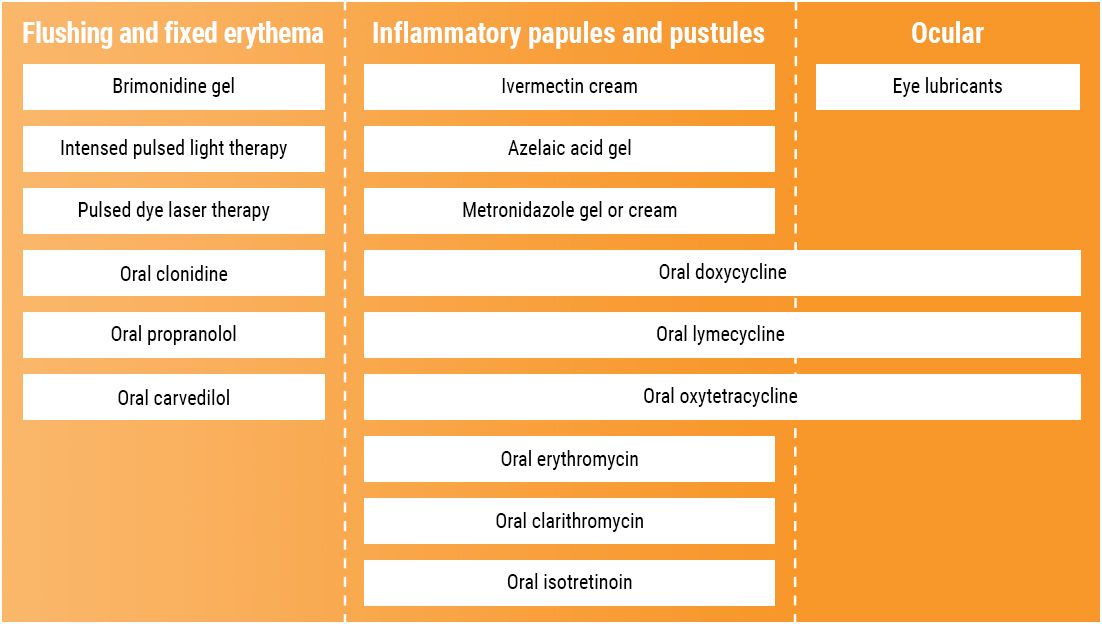
What drugs can be prescribed for rosacea?
Treatment summary19,22,25,28

Treatment summary19,22,25,28





Conclusion

The management of inflammatory skin conditions requires more than just symptom and disease control. Living with an inflammatory skin condition has a major impact on patients’ self image, confidence, self-esteem and mental wellbeing.
Acne, eczema, psoriasis and rosacea are visible and debilitating conditions, which are often associated with anxiety and depression. Optimal management of inflammatory skin conditions should take a holistic and patient-centred approach that alleviates symptoms, reduces flare-ups and addresses the psychological burden of living with the disease.
Useful links
Follow the links below for more information and resources about inflammatory skin conditions available on the MIMS website.
MIMS dermatology resources
Table: Emollients containing urea
Table: Emollients, potential skin sensitisers as ingredients
Table: Topical steroids, comparison of potencies and formulations
Table: Topical steroids, potential skin sensitisers as ingredients
References

1. British Skin Foundation. Know your skin. Last accessed November 2023.
2. All-Party Parliamentary Group on Skin. Mental health and skin disease. 2020.
3. Dreno B, Amici JM, Demessant-Flavigny AL et al. The impact of acne, atopic dermatitis, skin toxicities and scars on quality of life and the importance of a holistic treatment approach. Clin Cosmet Investig Dermatol 2021; 14: 623–32.
4. Misery L, Taïeb C, Schollhammer M et al. Psychological consequences of the most common dermatoses: data from the Objectifs Peau Study. Acta Derm Venereol 2020; 100(13): adv00175.
5. Zhang XJ, Wang AP, Shi TY et al. The psychosocial adaptation of patients with skin disease: a scoping review. BMC Public Health 2019; 19(1): 1404.
6. National Eczema Society. Stress and eczema. Last accessed November 2023.
7. Balieva F, Schut C, Kupfer J et al. Perceived stress in patients with inflammatory and non-inflammatory skin conditions. An observational controlled study among 255 Norwegian dermatological outpatients. Skin Health Dis 2022; 2(4): e162.
8. National Rosacea Society. Rosacea patients sound off on stress. Last accessed November 2023.
9. Hu S, Anand P, Laughter M et al. Holistic dermatology: an evidence-based review of modifiable lifestyle factor associations with dermatologic disorders. J Am Acad Dermatol 2022; 86(4): 868–77.
10. Reich A, Wójcik-Maciejewicz A, Slominski AT. Stress and the skin. G Ital Dermatol Venereol 2010; 145(2): 213–9.
11. Richard MA, Paul C, Nijsten T et al. Prevalence of the most common skin diseases in Europe: a population-based study. J Eur Acad Dermatol Venereol 2022; 36 (7): 1088–96.
12. Primary Care Dermatology Society. Acne vulgaris. Last updated May 2023.
13. NHS. Acne. Last reviewed January 2023.
14. NHS. Atopic eczema. Last reviewed December 2019.
15. NHS. Psoriasis. Last reviewed April 2022.
16. NHS. Rosacea. Last reviewed March 2023.
17. Primary Care Dermatology Society. Rosacea. Last updated November 2022.
18. Zhou C, Vempati A, Tam C et al. Beyond the surface: a deeper look at the psychosocial impacts of acne scarring. Clin Cosmet Investig Dermatol 2023; 16: 731–8.
19. NICE. Acne vulgaris: management. NG198. Last updated May 2023.
20. Allergy and Asthma Network. What is the allergic march? Last accessed November 2023.
21. Allergy UK. The mental health impact of living with atopic eczema. January 2022.
22. NICE. Atopic eczema in under 12s: diagnosis and management. CG57. Last updated June 2023.
23. Psoriasis Association. About psoriasis. Last reviewed March 2019.
24. Primary Care Dermatology Society. Psoriasis: an overview and chronic plaque psoriasis. Last updated June 2023.
25. NICE. Psoriasis: assessment and management. CG153. Last updated September 2017.
26. Garshick MS, Ward NL, Krueger JG et al. Cardiovascular risk in patients with psoriasis: JACC review topic of the week. J Am Coll Cardiol 2021; 77(13): 1670–80.
27. British Skin Foundation. Rosacea. Last accessed November 2023.
28. Primary Care Dermatology Society. Rosacea – primary care treatment pathway. Last reviewed October 2019.
Published by Haymarket Media Group Ltd, Bridge House, 69 London Road, Twickenham, TW1 3SP
You acknowledge that whilst Haymarket endeavours to ensure that information on this site is accurate and complete at the time of first publication, it is provided only for general information, is not intended to address your particular requirements and does not constitute any form of advice or recommendation by Haymarket. You acknowledge that the information on this site does not necessarily reflect the views and opinions of Haymarket, that such information should not be relied upon by you in making (or refraining from making) any specific investment or other business, professional or personal decisions and that you should seek independent professional advice before making any such decision. You also acknowledge that views and opinions expressed in content submitted by third party contributors are views and opinions of the authors of that content and not Haymarket’s views and opinions.
©2023 Haymarket Media Group Ltd.


